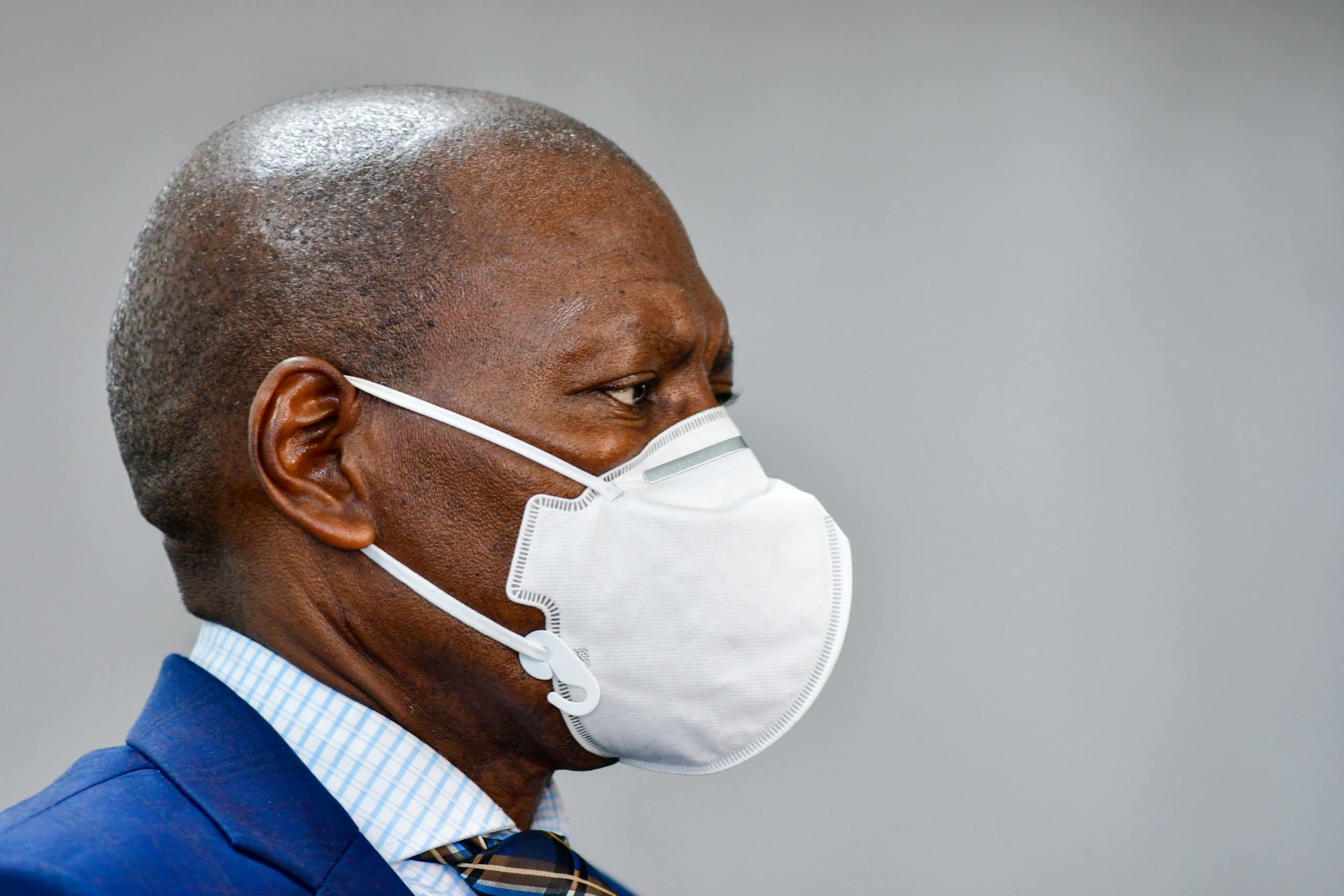
What a year it has been! In this mid-November interview with South Africa’s health minister Dr.Zweli Mkhize, he dwells on the early days of the pandemic and the country’s response, and the opportunities that have arisen.
Q. What do you think are some of the contributing factors to Africa having a relatively low caseload in comparison with other parts of the world?
A. While there are no definitive answers for this yet, there are several hypotheses I have with regards to this. Firstly, Africa had most of its initial cases come from various parts of the world, in particular Europe. As soon as the initial onset of the virus was identified correctly, international borders were closed. This meant that there was a significant decrease in imported cases and the focus could be shifted to cases being transmitted internally. This issue then in turn affected the number of cases. South Africa, for example, has an estimate of around 21 million international flyers per annum, however once this number was decreased; it played a significant role in decreasing the rate of spread. This also happened in Ethiopia and Kenya and had the same effect in reducing the rate of spread in their respective countries.
The second hypotheses I have relates to the intrinsic social systems that exist within the continent. The difference we have to more developed countries is that we have grassroot workers who go around and inform communities. This is the system we have used when dealing with other crises such as HIV, malaria and so on. The utilization of this system has proven itself to be consistently beneficial, especially given that universal health is not our strength.
Another theory, which has scientific grounding, is the presence of sunshine and the time it takes for the decomposition of the virus and given the theories around this, sunshine may well be a factor which impacts on the survival or life-span of the virus.
Loading...
The demographics of the continent have also played a role as Africa has a significantly skewed younger population. This group is affected less by the virus and rarely show symptoms or they experience very mild symptoms which could have also been a factor.
Lastly, testing could also prove to be a factor and as with other parts of the world, provides an estimation of the positive cases which may well be bigger than the figures show due to people within the population being asymptomatic and therefore not realizing that they need to be tested. For example, antibody tests carried out in certain regions indicated that antibodies were present but they had not tested positive for the virus or had not gone in to be tested due to little or no display of symptoms.
All of this however does require more research, as the points I’ve raised are anecdotal and still require more evidence from the science community.
Q. According to CDC Africa, the southern parts of Africa currently have over 800,000 Covid-19 cases [as of mid-November], higher than any other region within Africa. What do you think are some of the possible reasons for this?
A. Within the southern region, South Africa is responsible for around 90% of these positive cases. I think the social dynamics and metropolitan social life in South Africa would probably be a significant contributor.
The increasing numbers of cases, which were mainly imported, means that South Africa has quite a noticeable relation to the Western capitals that have been hard hit and because of the mode in which the virus reached our shores, we ended up with a high number of imported cases and at the same time, because of a more metropolitan lifestyle, we as a country, ended up with a much higher increase.
That then explains why South Africa has got higher numbers because as soon as we closed our borders to international travelers and our numbers began to be driven by internal transmission, we saw the rate of infection begin to slow, much like it did for other countries within Africa.
Q. South Africa is also renowned for its spirit of Ubuntu; do you think this has played a role in how the nation has approached overcoming this pandemic?
A. I think the element of Ubuntu probably works in the context of our community networks as people go out and use their existing social networks and understanding to try and prevent infection in others. It does tend to be a mixed bag as these social networks can also be used as a means to spread infection when not taking the proper precautions but it’s a factor you can’t completely rule out and needs more research.
Q. One thing that has come through is how efficiently the clinical trial process of vaccines can be expedited… Do you think these enhanced methods of management could be applied to other clinical trial processes such as HIV vaccine trials?
A. I think the innovations are very encouraging if you take into account their ability to carry out some phases in parallel to each other. This means that they were able to cover more ground with their research at a quicker pace and it is being done more efficiently than it has been done in the past. I think the lessons that have come through for the larger scientific community is that it is possible to expedite certain processes within the phases of trial research.
Concern for safety has arisen as a result of how quickly these trials have happened but should these vaccines prove their success in their final phases, then these new methods are a breakthrough as it has provided methods for safe and efficient clinical trials and definitely has applications to other vaccine trials within other fields of virology.
Q. South Africa is currently the only African country to be conducting clinical trials with Kenya awaiting final approval from internal processes and Uganda’s Virus Research Institute looking to collaborate with the Imperial College of London. What do you think needs to be done for Africa to become more of a clinical trial hub?
A. I think that the Africa CDC has the potential to play a vital role in this sphere as there is the potential to create a strong network of biomedical and biotechnological experts wherein various levels of expertise in different fields are able to collaborate on a single platform. This is so the level of knowledge and information sharing is more or less equal across various countries.
This will assist in creating a clinical trial hub within Africa. If you have specialists and experts within a specific field and have them in communication with each other, it creates collaboration which brings about new ideas on what needs to be done within clinical trials. If this then forms part of a network coordinated through the Africa CDC, you can then have the African CDC assist this process by acting as a base of support for countries willing to participate in these clinical trials and it allows for this to be done without needing to reinvent the wheel.
This means utilizing what’s available and getting the necessary support so you could, for example, have collaboration between the African CDC and all the current Covid-19 vaccine research institutions and this could provide a platform for trials to occur. Early discussions could look at the strengths of each research institute in each African country and evaluate who can rise to the occasion and who cannot, who could carry out a portion of the study and then be partnered with another country to carry out the other portions.
Once this platform is established, it provides the possibility for these African research institutes within various countries to apply and allows for assistance from African CDC in the form of resources and expertise, should any of these institutes be allowed to conduct a clinical trial. This should be the direction that the future takes.
The Covid-19 pandemic has proven this is possible as a pool of experts in various fields was created and was shared with the African CDC, so the teams within the CDC who are working on the Covid-19 pandemic consists of specialists who have all come from different countries and are from different disciplines. This is a good start to increasing clinical trials, as should these teams be enhanced and efforts towards collaboration are intensified, particularly across disciplines. This will then allow for them to communicate with other specialists and experts within various institutions across the globe.
Q. With organizations such as COVAX attempting to ensure vaccines reach every part of the globe, when do you foresee the vaccine reaching Africa and how do you think distribution of the vaccine should work?
A. This is an interesting topic and I can only speculate here as Pfizer foresees the progress with their vaccine reaching approval by the end of this year and getting a license to begin production. South Africa as a country would like to be a part of this success and therefore distribution can occur through initiatives such as COVAX, which in itself will look to utilize these vaccines as they become available.
Johnson & Johnson is looking at completing at the end of this year and possibly starting production of their vaccine around May. Now again, the need is to ensure that platforms such as COVAX also receive this vaccine as it becomes available.
The key challenges here are availability of financial resources to ensure that these vaccines are paid for; this is unaffordable to some countries, especially in Africa. Therefore, some countries on the continent will have no choice but to wait for humanitarian efforts from the likes of COVAX and CEPI.
There is also the collaboration of financial institutions such as the World Bank who are willing to provide support to some countries to ensure that they also have access. This will be a continuous effort to ensure that no country gets left behind and everyone is effectively immunized against Covid-19.
Q. Do you think there are protocols within the NHI that could have assisted with the free and fair distribution of vaccines within South Africa?
A. If NHI was currently an active entity within South Africa, this would have ensured that the total availability of these vaccines would have been secured through NHI protocols for funding, however given the current circumstances; everyone will now receive the vaccine according to their need and the criteria that has been set out by the country.
Certainly, the NHI would have assisted with the distribution of a vaccine. This, however, does not mean that we are unable to obtain access to a vaccine as government is still involved in procurement. We [government] are currently examining possible ways to ensure that the vaccine reaches everyone who truly needs it first.
Q: What applications does the NHI have to a pandemic such as Covid-19?
A: The fundamental point here is resilience and sustainability of the South African health system and that there is a strong foundation. If the foundation is strong, a pandemic such as this [Covid-19] becomes easier to manage. All of these points ensure the delivery of quality healthcare for all South Africans and the NHI becomes the platform from which a crisis response is formulated.
This system also ensures that the healthcare being received is the same in both rural and urban areas and should medical assistance be required, it is given without any compromises on the quality and speed at which these services are received. In a pandemic, this quality of care is essential in making sure it is properly treated no matter what the environment.
The key issue is ensuring that the NHI allows us to build an unshakeable foundation for the South African health service with good infrastructure and an abundance of human resources, adequate supplies of medical and technological devices and sufficient health information and promotion systems. All of which should be able to service all South Africans.
When a crisis such as the coronavirus occurs, we should then be able to utilize this system to allow a quick and efficient response and therefore ensure that those who require urgent attention have received it. We can also use the functions within this system to ensure the rest of the population has been adequately informed to ensure their safety.
Q: Do you think with resources being directed to the pandemic that it then forestalls on when the NHI becomes a viable option to the South Africa public?
A: I think the approach we take to a pandemic should not be a matter of ‘an either, or’ situation, the approach should focus simultaneously on our response to a pandemic like Covid-19, and the approach that allows us to move closer to using a universal health cover approach.
It then becomes a question of infrastructure systems used to manage the Covid-19 pandemic and that these additions to existing infrastructure not being dismantled after it has served its purpose. It should instead, be absorbed into existing infrastructure for future use.
Therefore what this pandemic has done is accelerate the creation of some infrastructure that will bring us closer to implementing the NHI. The second area it has impacted on is human resources; we will use this time to further expand on our pre-existing human resource pool which is part of securing South Africa in the future against crises such as the Covid-19 pandemic.
It has also moved forward collaborations and partnerships between the public and private health sector and basic agreements have begun to be reached on how to approach health-related issues going forward. Access to some private hospitals by public sectors was also given based on the needs of the public sector which included accommodations for costs, the quality of care that was received and so on.
So there have been opportunities that have arisen from the pandemic and the need for investment into the future of NHI has become apparent.
Q. With unified healthcare being a success in countries such as Brazil and Canada, do you think there are any lessons South Africa could take from them?
A. I think there’s only lessons to be learned from countries with a universal healthcare system; that we cannot wait any longer for the implementation of NHI as it provides healthcare to the areas where it is needed most.
Q. Lastly, do you have any concerns around the implementation of NHI?
A. I think this pandemic has shown us that circumstances don’t matter and shouldn’t forestall something this important. The pressure put on health resources by the Covid-19 pandemic and the impact it has had on the economy has slowed down the speed with which the NHI could have been implemented.
However, this does not mean that it should not still proceed, it means understanding that the current situation that we are in has placed constraints on certain aspects of the economy and this in turn has had an impact on the implementation of the NHI.
However, other countries have never looked at their wealth or state of economy when implementing a universal health system, this time with all these constraints is when implementing NHI is most essential and part of this is building on the infrastructure and systems that were successful.
So what NHI is now and what it can be in the future has to be taken into account as this is dependent on the available resources and look at how we can maximize the resources that are available.
Loading...